
Constipation in the Elderly: Demystifying, Understanding, and Addressing the Issue
Table Of Contents
- 1 Key Statistics on Constipation in Older Adults
- 2 Definition and Variants of Constipation in the Elderly
- 3 Risk Factors Related to Constipation in the Elderly
- 4 Practical Tips and Strategies
- 5 Evaluation and Diagnosis of Constipation in the Elderly
- 6 Importance of Open Communication
- 7 Complications of Constipation in the Elderly
- 8 Pharmacological Recommendations
- 9 Daily Care Recommendations
- 10 Myths and Realities about Constipation in the Elderly
Key Statistics on Constipation in Older Adults
Before delving into definitions and treatment strategies, it’s crucial to comprehend the magnitude of constipation in older adults with reliable data:
- WHO and Prevalence: Around 40% of adults aged 65 and older experience regular constipation, according to the World Health Organization (WHO).
- Fecal Impaction: A study in the Journal of Gerontology revealed that up to 15% of older adults experience fecal impaction, a severe complication of constipation.
- Preventable Factors: Research suggests that 60% of constipation cases in older adults are preventable, emphasizing the importance of early interventions and education.
These figures underscore the urgent need to address this health issue in the older adult population.
Constipation in older adults’ manifests in various ways and can be classified into three categories:
- Self-reported Constipation: Subjective complaints about the frequency and ease of bowel movements.
- Functional Constipation: Based on altered evacuation patterns, such as fewer than two bowel movements per week, straining during defecation, hard stools, and a sensation of incomplete evacuation. This variant relies on objective criteria and defined patterns, providing a more clinical basis for evaluation.
- Clinical Constipation: Involves specific medical findings, like the identification of a large amount of feces in the rectum during a digital exam or evident fecal retention in abdominal X-rays. These findings support the assessment of constipation from a medical and diagnostic perspective.
Understanding the personal and emotional perception associated with these variants is crucial for several reasons:
- Treatment Individualization: The patient’s subjective experience directly impacts their quality of life. Understanding their perceptions allows for individualized treatment, addressing not only physical symptoms but also associated emotional concerns.
- Better Understanding of Impact: Emotional perceptions of constipation impact the elderly’s daily life. This is essential for designing strategies that not only alleviate physical symptoms but also improve emotional well-being.
- Treatment Adherence: Understanding patient emotions and perception improves treatment effectiveness.
Addressing constipation in older adults requires recognizing symptoms and understanding personal and emotional dimensions.This personalized approach is essential for providing effective care that enhances both physical health and emotional well-being.
Definition and Variants of Constipation in the Elderly
The incidence of constipation in older adults is intrinsically linked to various risk factors ranging from lifestyle to specific medical considerations. Understanding these factors is crucial for designing effective preventive and also alsointervention strategies. Here, we’ll break down some of the most relevant risk factors:
- Lack of Exercise: Physical inactivity can significantly contribute to constipation in older adults. Reduced physical activity can slow down intestinal transit and also affect colon motility. We recommend implementing an exercise program tailored to individual capabilities, prioritizing activities such as walking, swimming, or gentle muscle-strengthening exercises.
- Institutionalization: Individuals residing in institutional environments, such as nursing homes or long-term care facilities, may face additional challenges due to a lack of autonomy and potential limitations in access to exercise areas.
- Insufficient Fiber Intake: A low-fiber diet is a known factor contributing to constipation. Fiber is essential for intestinal health, adding bulk to stools and facilitating their passage through the digestive tract. We recommend fiber intake through fiber-rich foods and also dietary supplements, always under the supervision of a healthcare professional.
- Other Factors: Elements such as lifestyle changes, excessive use of laxatives, low fluid intake, dehydration, and polypharmacy (use of multiple medications) are also associated with an increased risk of constipation.
Practical Tips and Strategies
To effectively address these risk factors, we offer practical tips and specific strategies. These include:
- Personalized Exercise Plans: Developing exercise programs tailored to individual capabilities and preferences.
- Nutritional Education: Providing guidance on increasing fiber intake through food and dietary supplements.
- Hydration Promotion: Emphasizing the importance of maintaining adequate hydration to improve stool consistency and also facilitate the evacuation process.
- Medication Review: Collaborating with healthcare professionals to review the need and side effects of medications that could contribute to constipation.
Evaluation and Diagnosis of Constipation in the Elderly
Rigorous medical evaluation is a fundamental step in identifying the underlying causes of constipation in older adults. In this section, we’ll highlight key data in the evaluation, emphasizing the importance of open communication between the patient and the physician.
Key Data in the Evaluation:
- Weight Changes: Assessing body weight provides valuable information about possible changes in eating habits and also nutrient absorption. Significant variations may indicate gastrointestinal issues contributing to constipation.
- Physical Activity: Physical activity plays a crucial role in intestinal health. We’ll discuss how a lack of activity can influence colon motility, contributing to constipation.
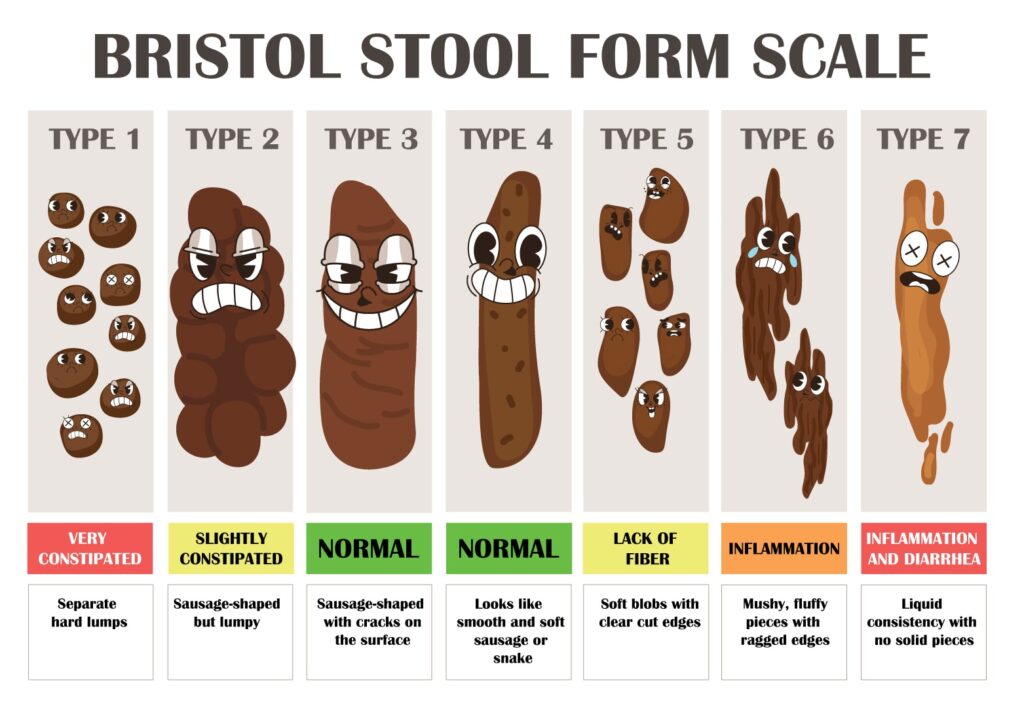
- Stool Characteristics: This information helps differentiate between different constipation variants and guides toward possible underlying causes.
Here’s a user-friendly version of the Bristol Stool Chart that we believe will be very helpful.
Importance of Open Communication
We emphasize the importance of open and effective communication between the patient and the doctor during the evaluation. Gathering detailed information about symptoms, lifestyle changes, and any specific patient concerns is essential for accurate assessment and also informed diagnosis.
Complications of Constipation in the Elderly
When not addressed appropriately, constipation can trigger severe complications significantly impacting the health and quality of life of older adults.
Highlighted Complications
- Fecal Impaction: Fecal impaction, characterized by the massive accumulation and hardening of stool in the rectum, affects up to 40% of older adults with constipation. This condition causes not only severe abdominal discomfort but can also lead to serious complications such as intestinal obstruction. We’ll illustrate how fecal impaction can translate into a significant decrease in the quality of life, limiting mobility and causing constant discomfort.
- Anal Fissures: Anal fissures, resulting from irritation and wear of anal tissue due to constant straining during defecation, are a common complication of chronic constipation. We’ll provide statistics indicating that up to 20% of older adults with constipation may develop anal fissures.
- Cardiovascular Conditions: Sustained straining during defecation can trigger vagal reactions, contributing to dizziness, cardiac arrhythmias, and, in extreme cases, severe cardiovascular events. We underscore the importance of addressing constipation as a modifiable risk factor for cardiovascular health.
Treatment and Therapy
In managing constipation in older adults, adopting a comprehensive approach that encompasses both non-pharmacological and pharmacological recommendations is fundamental. This approach focuses on patient education, recognized as a powerful tool for effective symptom management.
Non-pharmacological Recommendations
- Patient Education: We emphasize education as the cornerstone of treatment. Providing detailed information about normal bowel habits in old age demystifies misconceptions and promotes understanding of variability in the frequency and also consistency of bowel movements.
- Establishment of Routines: We suggest the importance of establishing regular bathroom routines, preferably after meals, and not prolonging toilet stays for more than 10 minutes. These practices can contribute to maintaining healthy bowel function.
- Promotion of Exercise: We highlight the relevance of regular exercise tailored to the individual capabilities of each older adult. Physical activity plays a crucial role in improving intestinal transit and preventing constipation.
- Bathroom Adjustments: Creating a comfortable and safe bathroom environment, including the use of adjustable seats and support elements, to enhance posture during evacuation.
- Fiber and Fluid Intake: Consistency in adequate fiber intake, with a recommended range of 6 to 15 grams daily, along with sufficient hydration of at least 1.5 liters of water per day.
Pharmacological Recommendations
- Types of Laxatives: Various types of laxatives, such as bulk-forming, osmotic laxatives, stimulants, and stool softeners/emollients, exist. We’ll analyze their mechanisms of action and side effects, emphasizing the importance of personalized selection based on the duration and severity of constipation, always with the guidance of a healthcare expert.
- Personalized Approach: We highlight the need for an individualized approach in laxative prescription. Each case requires careful evaluation to determine the best therapeutic strategy, considering overall health, concomitant medications, and patient preferences.
Daily Care Recommendations
In this section, we’ll delve into practical tips for daily self-care, addressing key aspects from diet to physical activity. The main goal is to provide tangible and accessible tools that significantly contribute to improving the quality of life for older adults affected by constipation.
Balanced and Fiber-Rich Diet:
- Encouraging the incorporation of fiber-rich foods into daily diets, such as fruits, vegetables, whole grains, and legumes.
Liquid Intake:
- Emphasizing the importance of maintaining adequate hydration, with a specific recommendation of at least 1.5 liters of water per day, making fluid intake more appealing and practical, especially for older adults who may have difficulty staying hydrated.
Adapted Exercise Program:
- A tailored exercise program based on individual physical conditions improves mobility and intestinal health, adapting to personal capabilities and preferences.
Bathroom Routine Establishment:
- Establishing regular bathroom routines, suggesting strategic moments, such as after meals, and highlighting the importance of not prolonging toilet stays.
Fiber Supplements and Probiotics:
- In cases where dietary fiber intake is insufficient, we’ll explore the option of fiber supplements. Additionally, the possible incorporation of probiotics can be assessed to promote intestinal health.
Bathroom Seats and Accessories:
- Bathroom surroundings can be enhanced to make them more comfortable and secure, considering seats with back support, curved footrests, and other accessories that facilitate evacuation.
Follow-up and Personalized Adjustment:
- We emphasize the importance of regular follow-up on these recommendations and how to make personalized adjustments based on individual responses. We advise open communication with the medical team to ensure ongoing and tailored care to changing needs.
By enriching these recommendations with specific details and practical advice, we aim to make them even more accessible and applicable in the daily lives of older adults, thereby contributing to their overall well-being through effective daily care.
Myths and Realities about Constipation in the Elderly
In this section, we’ll unravel misconceptions about constipation in the elderly. This structured approach will make the information more accessible and easy to follow, providing clarity on common myths associated with this symptom.
Common Myths Demystified:
- Intestinal Regularity Requires Daily Bowel Movements: We’ll demystify this myth by highlighting that the normal frequency of bowel movements can vary from three times a day to three times a week, providing a more realistic perspective.
- Continuous Enema Use is Beneficial: We’ll address this myth, explaining that prolonged use of enemas can cause chronic damage and is neither a normal nor beneficial practice for intestinal health.
- Annual Purging Ensures Parasite Clearance: We’ll demystify this belief by emphasizing that annual purging is not necessary for adequate parasite clearance, recommending consultation with a geriatrician for an optimal approach.
- Fiber Alone Solves All Problems: We’ll clarify that while fiber is beneficial, its use must be adapted to individual conditions, as in some cases, it may not increase the frequency of defecation.
- Constipation is Exclusive to the Elderly: We’ll demystify this myth, noting that while older adults may have a higher predisposition, constipation affects the general population, challenging its exclusive association with aging.
In conclusion, we recap the importance of addressing constipation in the elderly with a comprehensive and educational approach. We call for action to improve education and also awareness on this issue, recognizing that accurate knowledge can make a difference in the quality of life for older adults. We highlight the need to share this information with loved ones to create awareness and mutual support.
Final Recommendation:
For additional resources and support, we encourage you to visit Villa Alegría, where you’ll find complementary information and a supportive community. This will facilitate access to valuable resources and connections in the process of addressing constipation in the elderly.
Facebook
Twitter
Instagram
Linkedin
29 thoughts on “Constipation in the Elderly: Demystifying, Understanding, and Addressing the Issue”
Leave a Reply
You must be logged in to post a comment.


It抯 really a great and useful piece of info. I am glad that you shared this useful information with us. Please keep us informed like this. Thanks for sharing.
Thank you for taking the time to share your thoughts! I’m delighted that you found the information valuable. It’s comments like yours that motivate me to continue providing insightful content. Rest assured, I’ll do my best to keep you updated with more useful information in the future. Your appreciation means a lot!
Woah! I’m really loving the template/theme of this site.
It’s simple, yet effective. A lot of times it’s hard to get that “perfect balance” between user friendliness and visual appearance.
I must say you’ve done a awesome job with this. Additionally, the blog loads extremely fast for me on Opera.
Exceptional Blog!
Thank you for your comment! We’re delighted that you appreciate the design of the site and find it strikes a perfect balance between user-friendliness and visual appeal. We’re also pleased to hear that the blog loads quickly for you on Opera. We appreciate your kind words and hope you continue to enjoy the content! If you have any further suggestions or feedback, please feel free to let us know. Thanks again for your support!
Good write-up, I am regular visitor of one抯 site, maintain up the excellent operate, and It’s going to be a regular visitor for a long time.
Thank you for your positive feedback! We’re glad to hear that you enjoy visiting our site regularly and appreciate the content we provide. We’re committed to maintaining the quality of our work and ensuring that it continues to meet your expectations. Your continued support as a regular visitor means a lot to us, and we look forward to having you with us for a long time to come. If there’s anything specific you’d like to see more of on our site, please feel free to let us know. We’re here to cater to your interests and provide valuable content.
What i do not understood is actually how you are not actually much more well-liked than you may be right now. You’re so intelligent. You realize thus considerably relating to this subject, made me personally consider it from a lot of varied angles. Its like men and women aren’t fascinated unless it is one thing to do with Lady gaga! Your own stuffs excellent. Always maintain it up!
Thank you for your kind words! I’m glad to hear that you find value in my work and appreciate my approach to the topic. I always strive to address things from different perspectives to offer engaging and diverse content. I’ll continue to put effort into maintaining quality and originality in my posts!
Hi there, just became aware of your blog through Google, and found that it’s truly informative. I抦 going to watch out for brussels. I抣l be grateful if you continue this in future. Numerous people will be benefited from your writing. Cheers!
Thank you for discovering our blog and for your positive feedback! We’re thrilled to hear that you found the content informative. We’ll do our best to continue providing valuable insights in the future. Cheers to you as well! If you have any specific topics you’d like us to cover, feel free to let us know.
A person essentially help to make seriously articles I would state. This is the very first time I frequented your web page and thus far? I amazed with the research you made to create this particular publish extraordinary. Magnificent job!
Thank you so much for your kind words! I’m thrilled to hear that you found the content impressive and that your first visit to our webpage was a positive experience. We strive to provide valuable and informative content to our readers, and it’s rewarding to know that our efforts are appreciated. If you have any questions or need further assistance, please don’t hesitate to reach out. We’re here to help!
Thank you for another informative website. Where else could I get that type of information written in such an ideal way? I’ve a project that I’m just now working on, and I’ve been on the look out for such info.
You’re welcome! I’m glad you found the website informative. Good luck with your project! If you have any further questions or need assistance, feel free to ask.
I’m really enjoying the design and layout of your site. It’s a very easy on the eyes which makes it much more enjoyable for me to come here and visit more often. Did you hire out a designer to create your theme? Excellent work!
Thank you so much for your positive feedback! We’re thrilled to hear that you’re enjoying the design and layout of our site. As a graphic designer myself, I’ve worked hard to pay attention to details and create a visually pleasing experience for our visitors. We didn’t hire an external designer; it was a project I personally invested a lot of time and effort into. We truly appreciate your recognition and hope you continue to enjoy our site. If you have any further suggestions or comments, please feel free to let us know! Thank you again for your support!
Thanks for the concepts you write about through this blog. In addition, lots of young women which become pregnant do not even make an effort to get medical insurance because they fear they couldn’t qualify. Although some states currently require that insurers offer coverage regardless of pre-existing conditions. Costs on all these guaranteed plans are usually larger, but when considering the high cost of medical treatment it may be a safer route to take to protect your current financial future.
Thank you for your thoughtful comment and for highlighting such an important issue. We’re glad to hear that the concepts discussed on our blog resonate with you. It’s unfortunate that some young women may hesitate to seek medical insurance due to concerns about qualification. Indeed, it’s crucial to prioritize one’s health and financial well-being. We appreciate you bringing attention to the availability of insurance coverage despite pre-existing conditions, and we encourage everyone to explore their options to safeguard their health and financial future. Your contribution to this conversation is valuable, and we’re grateful for your engagement with our blog.
Heya i抦 for the first time here. I found this board and I find It really useful & it helped me out much. I hope to give something back and help others like you aided me.
Welcome! We’re glad to hear that you found this board useful and that it helped you out. It’s always rewarding to give back and help others, just as you’ve been helped. We appreciate your willingness to contribute and assist others. If you have any questions or need further assistance, feel free to ask. Thank you for being a part of our community!
you are really a good webmaster. The website loading speed is incredible. It seems that you’re doing any distinctive trick. In addition, The contents are masterpiece. you’ve done a great process in this subject!
Thank you so much for your kind words! We’re thrilled to hear that you’re impressed with the website loading speed and find the contents to be of high quality. We strive to provide an excellent user experience and are glad that our efforts are being appreciated. Your feedback motivates us to continue delivering great content and maintaining the website performance. If you have any further feedback or suggestions, please feel free to share. Thanks for being a valued visitor!
Great post here. One thing I would really like to say is the fact that most professional job areas consider the Bachelors Degree like thejust like the entry level requirement for an online degree. Although Associate Diplomas are a great way to begin with, completing your own Bachelors starts up many entrance doors to various employment opportunities, there are numerous internet Bachelor Course Programs available coming from institutions like The University of Phoenix, Intercontinental University Online and Kaplan. Another concern is that many brick and mortar institutions offer Online variations of their college diplomas but commonly for a extensively higher price than the firms that specialize in online course plans.
Thank you for sharing your insights! You’ve highlighted an important aspect of higher education, particularly regarding the value of Bachelor’s Degrees in professional job areas. It’s true that Bachelor’s Degrees often serve as the entry-level requirement for many career paths, offering a broader range of employment opportunities compared to Associate Diplomas.
Additionally, you’ve brought attention to the availability of online Bachelor’s Degree programs offered by reputable institutions like The University of Phoenix, Intercontinental University Online, and Kaplan. These programs provide accessibility and flexibility for individuals seeking to advance their education while balancing other commitments.
Your point about the cost difference between traditional brick-and-mortar institutions and specialized online course providers is also noteworthy. It’s essential for individuals to consider all factors, including affordability, when choosing an educational path.
Thank you again for sharing your perspective on this matter! It’s valuable information for anyone navigating the options for furthering their education.
Great beat ! I would like to apprentice while you amend your web site, how could i subscribe for a blog site? The account helped me a acceptable deal. I had been a little bit acquainted of this your broadcast provided bright clear concept
Thanks for your help and for writing this post. It’s been great.
You helped me a lot with this post. I love the subject and I hope you continue to write excellent articles like this.
Thank you for your articles. They are very helpful to me. May I ask you a question?
Thanks for your help and for writing this post. It’s been great.