
Urinary Incontinence: A Significant Challenge for Geriatric Health
Urinary incontinence poses a significant challenge for geriatric health, impacting a sizable portion of individuals aged over 65. However, surprisingly, only a third of these patients seek medical help to address this issue. What are the reasons behind this reluctance? Psychosocial barriers, including feelings of shame and the pervasive belief that incontinence is an unavoidable aspect of aging, frequently impede the pursuit of effective solutions.

Urinary incontinence exerts a multifaceted impact on the quality of life of older adults, manifesting at various levels:
- Physical level: At the physical level, incontinence is associated with an increased risk of falls, urinary tract infections, and even skin lesions due to constant moisture. Additionally, it limits participation in physical activities, restricting mobility and autonomy.
- Psychological level: Loss of control over urinary function can trigger a decrease in self-esteem, anxiety, depression, and stress, negatively affecting emotional well-being.
- Social level: Incontinence contributes to social isolation, undermining social interactions and reducing participation in community activities, which can lead to feelings of loneliness and alienation.
Types and Clinical Presentations
Urinary incontinence presents in various forms, each with its distinctive characteristics:
- Urgency Incontinence: Characterized by urine leaks preceded by a sudden, uncontrollable urge to urinate, often associated with central nervous system disorders or underlying urological conditions.
- Stress Incontinence: In stress incontinence, activities that increase intra-abdominal pressure, such as coughing, sneezing, or laughing, trigger urine leaks. This type is more common in multiparous women, men post-prostatectomy, and individuals with obesity.

Comprehensive Geriatric Approach
When faced with urinary incontinence in older adults, a holistic approach led by geriatric professionals is crucial to optimizing outcomes. This approach includes:
- During a Comprehensive Evaluation, healthcare professionals conduct a thorough assessment to identify the type and possible causes of incontinence, which guides the treatment strategy.
- For Personalized Treatment, healthcare providers design individualized treatment plans that combine various interventions aimed at improving quality of life and, if possible, restoring continence.
- For Conservative Measures, healthcare providers recommend hygienic-dietary approaches, such as avoiding specific irritant beverages and foods, maintaining physical activity, and wearing comfortable, easily accessible clothing.
- Environmental Intervention involves making adjustments to facilitate bathroom access and the use of support devices, such as handrails and risers, to promote independence.
- In Palliative Therapies, comfort options, including absorbent products, are provided to minimize discomfort associated with incontinence and maintain skin integrity.
- Behavioral Modification teaches individuals techniques to restore bladder emptying patterns and enhance bladder control.
- In Pharmacological Treatment, healthcare providers may consider prescription medications in selected cases to address incontinence, always under medical supervision and while considering possible side effects in the older population.
- For Specialized Referral, healthcare providers will refer individuals to urology or gynecology specialists when necessary to evaluate surgical treatment options.
We should not perceive urinary incontinence in older adults as an inevitable or untreatable condition. With a comprehensive approach, ranging from conservative measures to pharmacological and surgical interventions, it is possible to significantly improve the quality of life of older patients and restore their autonomy and well-being. Overcoming psychosocial barriers and fostering a culture of openness and seeking medical help is essential to ensure that all individuals can enjoy a full and active life in their golden years.
Incontinence Affects Both Males and Females
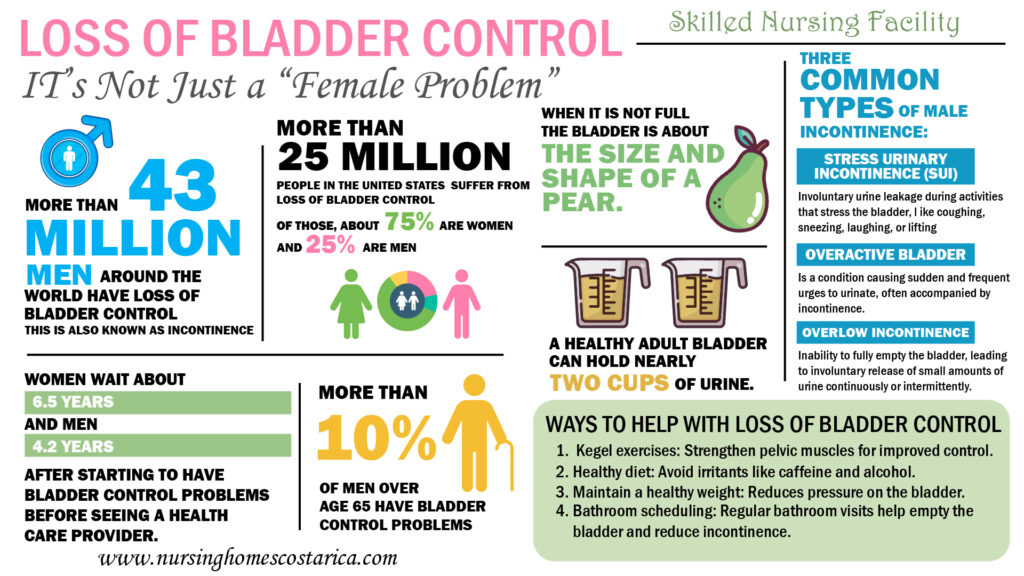
During Bladder Health Month, celebrated in November, the Urology Care Foundation (UCF) seeks to shed light on various health conditions affecting the bladder and urinary tract, including stress urinary incontinence, overactive bladder, and incontinence.
Despite many misconceptions, loss of bladder control affects both males and females. In fact, approximately 25 million Americans suffer from loss of bladder control (75% are women and 25% are men). During the month of November, the UCF urges patients to learn the facts and take an active role in their personal bladder health…
Sources:
This infographic highlights a fundamental fact: urinary incontinence does not discriminate by gender and can affect both males and females. By educating and raising awareness, we can dismantle the stigma surrounding this health issue, thereby promoting greater understanding and support for those affected by it.